Case of the Month - February 2021
A 61-year-old woman presented to the Emergency Room with nausea, vomiting, abdominal pain, diarrhea, myalgias, weakness, shortness of breath, and productive cough for a few days. Close family members had similar symptoms. Her past medical history was significant for hypertension, asthma, chronic obstructive pulmonary disease, hyperlipidemia, obesity, and obstructive sleep apnea.
She was hypotensive, tachycardic with atrial flutter, and hypoxic. Her chest X-ray showed diffuse infiltrates consistent with pneumonia and her SARS-CoV-2 PCR test was positive. She was admitted to the Intensive Care Unit for COVID pneumonia with acute respiratory failure and septic shock, where she was intubated. Her condition was complicated by ventilator-associated pneumonia caused by MRSA, and she was treated with vancomycin. After a week, she was extubated. She slowly continued to improve, but about 2 weeks after being extubated, she had several syncopal episodes with associated bradycardia, hypotension, hypothermia, diarrhea, and new leukocytosis. Blood cultures and urine were obtained and vancomycin and piperacillin-tazobactam were started. She became obtunded, developed a metabolic acidosis, and was intubated again. A chest CT scan showed worsening lung findings including ground glass infiltrates, interlobular thickening, bilateral pleural effusions, complete right lower lobe collapse, and partial left lower base collapse.
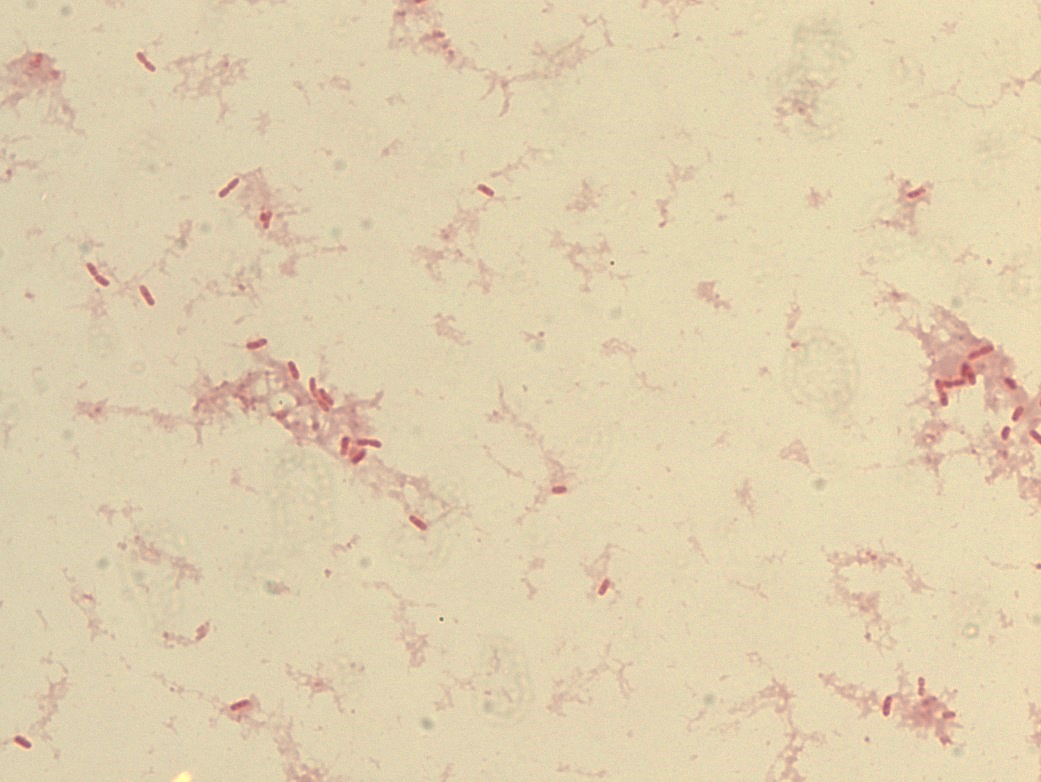
The organism shown below grew in two blood cultures. An oxidase spot test done from the colony was negative. What is this organism?