Esperanza Arias-Perez, Ph.D.
- Associate Professor, Department of Medicine (Hepatology)
- Associate Professor, Department of Pathology
Area of research
- Metabolic hepatic injury elating to pathobiology and treatment of fatty liver disorders, hepatic tumorigenesis and liver cancer progression.
Location
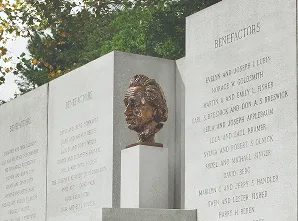
- Albert Einstein College of Medicine Jack and Pearl Resnick Campus 1300 Morris Park Avenue Ullmann Building 609A Bronx, NY 10461
Research Profiles
Professional Interests
We are interested in understanding the connection between pathological processes associated with age, and the malfunctioning of a cellular pathway involved in quality control and energy homeostasis known as autophagy. All the cells in the human body have surveillance systems that detect and eliminate damaged structures and toxic products. Our working hypothesis is that these surveillance mechanisms, including autophagy, become defective as organisms age and this results in accumulation of damage inside cells, which often leads to their functional failure and death. The ultimate goal of our studies is to devise interventions to repair or restore normal autophagic activity to increase the healthy years of life.
Cancer is also considered an age-related disease as the incidence of most cancers increases with age, rising more rapidly beginning in midlife. Hepatocellular carcinoma (HCC) remains one of the most prevalent and deadliest cancers. Recent studies suggest that nonalcoholic fatty liver disease (NAFLD) can be associated with approximately 15–50% of HCC “idiopathic” cases. NAFLD progresses slowly and can develop into NASH, liver cirrhosis, liver failure, and HCC. In addition to age, excessive weight and excess of insulin are also considered as risk factors of developing HCC in NASH.
Different systems are responsible for the maintenance of quality control and regulation of metabolic pathways in the liver, and its failure have been involved in hepatic pathology. We have evidence that malfunction of the surveillance protective system, known as chaperone-mediated autophagy (CMA), can be determinant in the progression of NASH into HCC. Our studies test the possible therapeutic value of modulating the activity of CMA as a novel therapeutic approach for this serious liver disorder.