News Releases
In the News
The Future of ART Regimens for HIV Is in Long-Acting Agents
Infectious disease physician, Barry S. Zingman, M.D. shares what to know about recent developments in antiretroviral therapies for HIV.
August 4, 2025
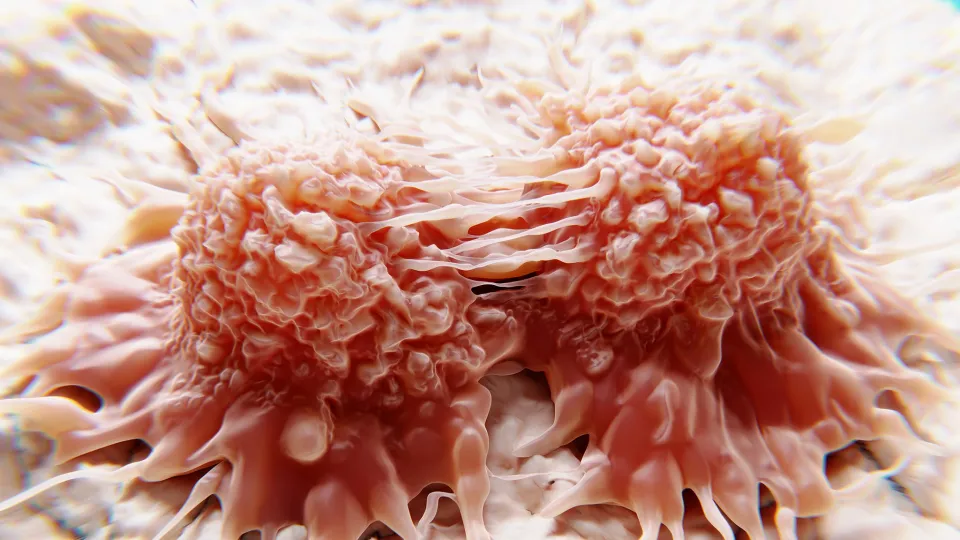
Viral Infections in the Lung Can Reactivate Dormant Cancer Cells
Cancer biologist Julio Aguirre-Ghiso, Ph.D., discusses his Nature study on respiratory viruses and metastasis.
July 30, 2025
Red Light Therapy Can Benefit the Skin, a Westchester Expert Explains
Cosmetic dermatologist, Kseniya Kobets, M.D., shares the benefits of red light therapy for a person’s hair and skin.
July 9, 2025
Header
Experts for Media
Header
Experts for Media
Research
September 17, 2025
September 16, 2025