Fetal Liver Research
Conditions Found that Promote Proliferation of Blood-Forming Cells in Fetal Liver
January 8, 2016—(BRONX, NY)—A study directed by Paul Frenette, M.D., is featured on the cover of today’s print edition of Science. In experiments involving mice, Dr. Frenette and his colleagues have solved a mystery surrounding the development of hematopoietic stem cells in utero. Dr. Frenette is professor of medicine and of cell biology and chair and director of Einstein’s Gottesman Institute for Stem Cell and Regenerative Medicine Research.

Paul Frenette, M.D.Researchers have long known that fetal hematopoietic stem cells (HSCs)—which ultimately give rise to adult blood cells—migrate during development from the dorsal aorta and placenta to the fetal liver, and later travel from there to the bone marrow. The Science article describes for the first time the conditions that promote HSC proliferation in the fetal liver.
Dr. Frenette collaborated in this study with Aviv Bergman, Ph.D., professor and founding chair of systems and computational biology. It provides evidence that pericytes (contractile cells that wrap around capillaries and venules) associate with the liver’s portal vessels (tributaries of the umbilical vein) to form a niche, or microenvironment, that promotes HSC proliferation in the fetal liver. This rapid expansion of HSCs contrasts sharply with their quiescence when HSCs later reside in bone marrow. Insights into this HSC fetal liver niche may lead to new ways of cultivating stem cells for transplantation. Their findings suggest that the expansion of HSCs during fetal development is governed by fractal geometries (repeating patterns that display at every scale) associated with the growing surface area of the portal vessel niche.
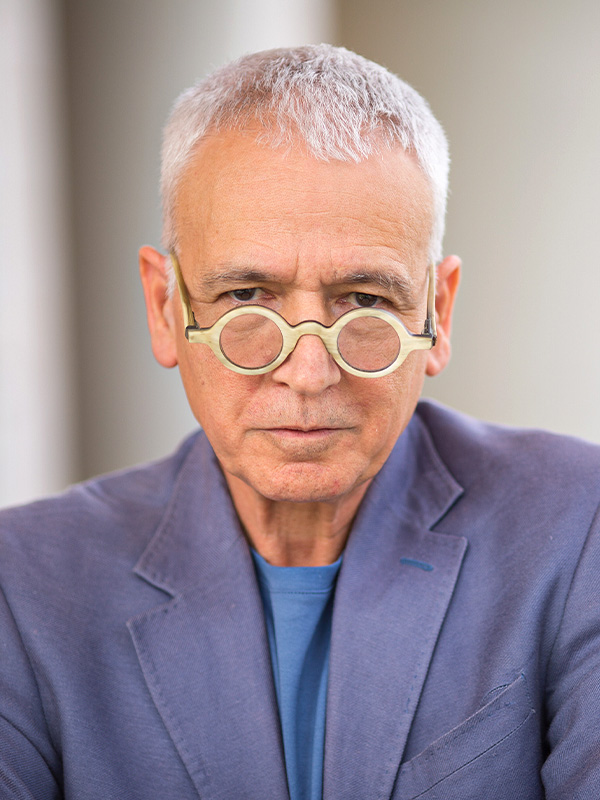
Aviv Bergman, Ph.D.The study was led by an M.D./Ph.D. student Jalal Khan. Other authors include Avital Mendelson, Ph.D., Yuya Kunisaki , M.D., Alexander Birbrair, Ph.D., Anna Arnal-Estapé, Ph.D., Sandra Pinho, Ph.D., Paul Ciero, M.S., Fumio Nakahara, M.D., Ph.D., all at the Gottesman Institute for Stem Cell and Regenerative Medicine Research , and collaborators Yan Kou, Ph.D., Avi Ma’ayan, Ph.D., and Miriam Merad, M.D., Ph.D., at the Icahn School of Medicine at Mount Sinai.
A leading stem cell and vascular biology researcher, Dr. Frenette joined Einstein from Mt. Sinai School of Medicine in July 2010, when he was named the first director of the Gottesman Institute. In studies published in Nature in 2010 and 2013, Dr. Frenette showed that HSCs pair up in the bone marrow with another type of stem cells, known as mesenchymal stem cells, which give rise to bone, cartilage, fat and other tissues, and that subsets of these cells are found in distinct blood vessels (arterioles and sinusoids) of the bone marrow where they differentially regulate HSC quiescence.
Dr. Frenette and colleagues showed in a 2013 Nature Medicine paper that macrophages in the bone marrow and spleen nurture the production of new red blood cells while they simultaneously clear aging red blood cells from the circulation—a finding that may lead to new therapies for conditions that cause abnormal red cell counts (e.g., hemolytic anemia and acute blood loss) and may aid recovery from chemotherapy and bone marrow transplantation. And in research on sickle cell disease published last September in Nature, Dr. Frenette found that using antibiotics to deplete the body’s microbiome may prevent acute sickle cell crisis and could offer the first effective strategy for warding off the disease’s long-term complications, such as organ failure.
In fiscal year 2014, Dr. Frenette received a five-year, $2.3 million National Institutes of Health renewal grant to continue his studies of the stem cell microenvironment. One of his new goals is to investigate how neural signals link the brain and the bone marrow by looking at two different ways that neural signals are transmitted to bone marrow.
Other Top Stories
9/11 World Trade Center Exposure Linked to Heart Disease Among NYC Firefighters
On Becoming a Physician: New Einstein Students Receive White Coats and Stethoscopes
Novel Therapy for Acute Migraine Shows Promise in Phase 3 Clinical Trial
First Complete Wiring Diagram of an Animal's Nervous System
Multimillion Dollar NIH Grant to Help Reduce Opioid Use & Get Care to People Who Need It
NIH Grant Funds $23 Million Study of Diseases Affecting People Living with HIV
New TAILORx Data Guides Adjuvant Therapy in Younger Breast Cancer Patients
Einstein Celebrates Its 61st Commencement
Bolstering Biopsies: Testing Patients' Individual Cells to Guide Treatment


Tablet Blog