Aging Research
Living Longer Associated with Living Healthier, Study of Centenarians Finds
July 5, 2016—(BRONX, NY)—Research has shown that the human lifespan has the potential to be extended. But would this merely mean people living longer in poor health? The upbeat findings from a new study in the Journal of the American Geriatrics Society indicate that those extra years could well be healthy ones. In a study of nearly 3,000 people, the onset of illness came decades later in life for centenarians than for their younger counterparts.
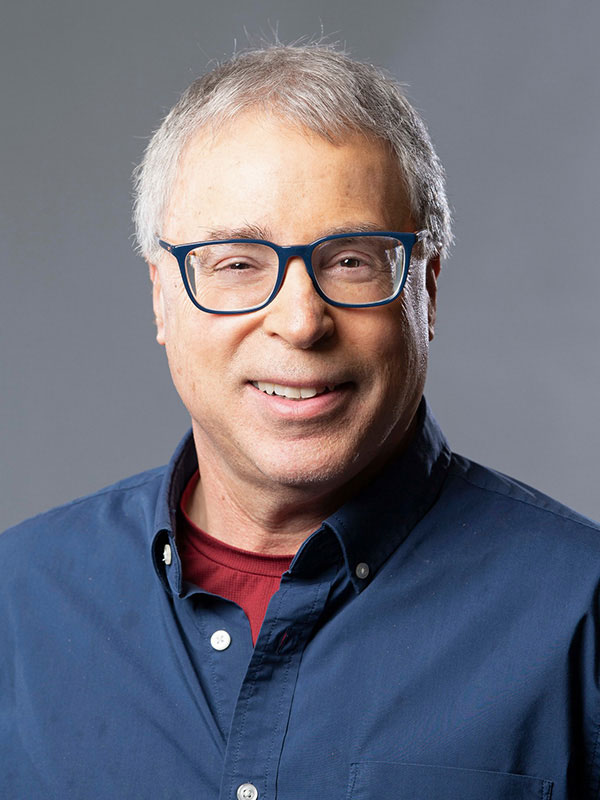
Nir Barzilai, M.D.“Most people struggle with an ever-increasing burden of disease and disability as they age,” said study leader Nir Barzilai, M.D., professor of medicine and of genetics at Albert Einstein College of Medicine, director of Einstein’s Institute for Aging Research, and attending physician at Montefiore. “But we found that those who live exceptionally long lives have the additional benefit of shorter periods of illness – sometimes just weeks or months – before death.”
The researchers looked at the health status of centenarians and near-centenarians enrolled in two ongoing studies: the Longevity Genes Project (LGP) and the New England Centenarian Study (NECS). Since 1998, Dr. Barzilai and colleagues have conducted the LGP, which recruits healthy, independently living Ashkenazi Jewish people 95 and older from the northeastern United States. For comparison, the LGP includes a group of Ashkenazi Jewish individuals who do not have a parental history of longevity. The NECS began in 1994 as a study of all centenarians living in eight towns near Boston and was later expanded to include participants from North America generally as well as England, Ireland, Australia and New Zealand. The NECS comparison group consisted of people aged 58 to 95.
"Most people struggle with an ever-increasing burden of disease and disability as they age, but we found that those who live exceptionally long lives have the additional benefit of shorter periods of illness – sometimes just weeks or months – before death."
– Nir Barzilai, M.D.
This study compared (1) the health status of 483 long-lived LGP participants with 696 LGP comparison individuals 60-94 years old, and (2) the health status of 1,498 long-lived NECS participants with 302 NECS comparison subjects aged 58-95. For both sets of comparisons, the researchers looked at the ages at which individuals developed five major age-related health problems: cancer, cardiovascular disease, hypertension, osteoporosis and stroke. Analysis revealed a consistent pattern of delayed onset of illness in the LGP and NECS centenarian groups compared to their respective comparison groups.
For example, for the long-lived NECS individuals, cancer didn’t afflict 20 percent of men until age 97 and women until 99. In contrast, 20 percent of NECS comparison participants had developed cancer by age 67 in men and 74 in women. Results were similar for the LGP: for the long-lived LGP participants, the age at which 20 percent had developed cancer was delayed to 96 for both sexes. But cancer had affected 20 percent of LGP control-group males by age 78 and control-group females by 74.
Despite their genetic, social and cultural differences, the long-lived LGP and NECS participants proved markedly similar with respect to major illness: Compared to younger comparison groups, their onset of major age-related disease was delayed, with serious illness essentially compressed into a few years very late in life. The findings suggest that discoveries made in one group of centenarians can be generalized to diverse populations. And they contradict the notion that the older people get, the sicker they become and the greater the cost of taking care of them.
The study is titled “Compression of Morbidity Is Observed Across Diverse Cohorts with Exceptional Longevity.” In addition to Dr. Barzilai, other Einstein authors were Sofiya Milman, M.D., and medical student Khadija Ismail. Additional authors were Paola Sebastiani, Ph.D., Stacy Andersen, Ph.D., and Lisa Nussbaum of Boston University School of Public Health, Boston, MA; and Thomas Perls, M.D., M.P.H., of Boston University School of Medicine, Boston, MA.
This research was funded by National Institutes of Health, including the National Institute on Aging (P01AG021654 and RO1 AG 042188-01) and the Clinical and Translational Science Awards from the National Center for Advancing Translational Sciences (UL1 TR001073, TL1 TR001072, KL2 TR001071). The authors report no conflict of interest.
Other Top Stories
9/11 World Trade Center Exposure Linked to Heart Disease Among NYC Firefighters
On Becoming a Physician: New Einstein Students Receive White Coats and Stethoscopes
Novel Therapy for Acute Migraine Shows Promise in Phase 3 Clinical Trial
First Complete Wiring Diagram of an Animal's Nervous System
Multimillion Dollar NIH Grant to Help Reduce Opioid Use & Get Care to People Who Need It
NIH Grant Funds $23 Million Study of Diseases Affecting People Living with HIV
New TAILORx Data Guides Adjuvant Therapy in Younger Breast Cancer Patients
Einstein Celebrates Its 61st Commencement
Bolstering Biopsies: Testing Patients' Individual Cells to Guide Treatment


Tablet Blog