At the heart of any residency experience is the patients. At Wakefield, you will learn from patients who reflect the diversity and complexity of the Bronx. You will be grounded in “bread and butter” medicine but will be surprised by the unusual conditions and situations you encounter. You will truly be your patients’ primary provider and advocate.
Inpatient
Your Inpatient Team: each ward team (day team) is composed of a PGY2 or PGY3 resident, 2 interns and medical students. The night medicine teams are not traditional night float teams; they participate in teaching and bedside rounds each day and will present patients they admit directly to the day team. Each team is capped at 16 patients, to allow adequate time for patient care and learning. You and your team are the primary physicians for your patients; your supervising attending is there to guide and teach but we believe that your growth depends on progressive independence, i.e. supervised autonomy.
Your Cardiac Telemetry Team: this is a smaller inpatient ward team with 1 resident and 1 intern taking care of up to 12 patients who require more intensive cardiology specific care. The team is led by a full-time cardiologist.
Hospitalist rotation: all PGY3 residents participate in our Hospitalist rotation. This rotation is designed to prepare you for post-residency work (whether as a generalist or fellow) by allowing you to work with more independence while still being supervised by our faculty.
Geographic Units: all your patients are located together on a single unit, minimizing the time spent “commuting” within the hospital and maximizing your efficiency on work and teaching rounds. You will work collaboratively with your Interdisciplinary Team (nursing, social work, case managers and physical therapists) on the unit.
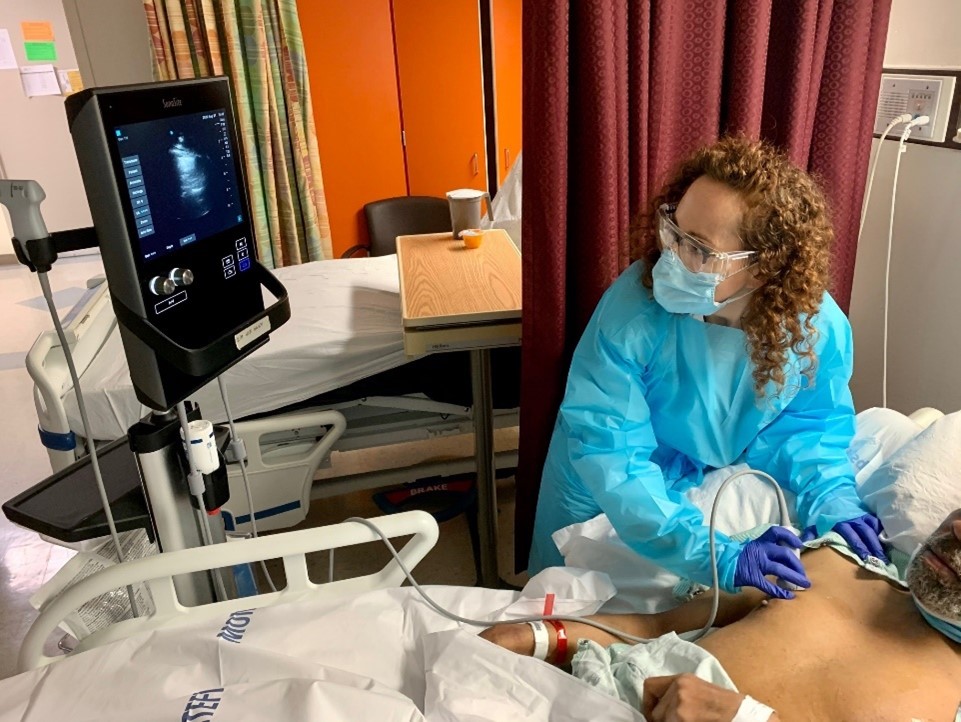
Point of Care Ultrasound (POCUS)
ICU Rotation: The Wakefield ICU is a 16-bed, closed ICU where all residents and interns rotate every year. The team consists of upper-level residents and interns, a fellow, and a critical care attending is present onsite 24/7. The entire team participates in rounds to deliver evidence-based care and the curriculum includes bedside POCUS, procedure rounds, journal clubs, and opportunities to participate in quality improvement projects.
Non-Wakefield rotations: all residents participate in an inpatient Oncology rotation at the Moses Campus and a Cardiac Care Unit (CCU) rotation at the Weiler Campus.
Subspecialty Electives: electives are available in all the medical subspecialties and Neurology and take place on the Wakefield Campus.
Off-site Elective: all PGY1s have the opportunity to apply for a PGY2 off-site clinic or research elective at any Montefiore Medical Center site to gain additional experience. Examples of previous electives include: advanced heart failure, hepatology, patient safety, transplant ID and palliative care.
Emergency Medicine: all PGY3s spend a total of 4 weeks in our Level 2 Emergency Department.
Point of Care Ultrasound (POCUS): Throughout the year there will be a core lecture series on point-of-care ultrasound technique and image interpretation that is led by Dr. Joseph Hong, Associate Program Director. The purpose of these lectures is to familiarize all house staff with the principles of ultrasound (I.e., “knobology”), the standard bedside ultrasound views taken of the heart, lungs and abdomen, and goal-directed binary interpretation of these views.
For hands-on experience, POCUS techniques will be taught at bedside during the Medicine consult rotation with POCUS faculty and the consult resident. Teaching will be done one-to-one using patients admitted to the hospital as examples of normal and abnormal findings. Residents will also have exposure to POCUS image acquisition and interpretation during their ICU rotations and while serving on the critical care consultation service.
Outpatient
![]()
Clinic Rotation: your outpatient clinic is located at the Wakefield Ambulatory Care Center, just 1 block away from the hospital. The clinic experience allows you to develop skills in outpatient medicine, with more focus on preventive healthcare, chronic disease management, and longitudinal relationships with your patients. In addition to building your personal patient panel that you will follow regularly for continuity of care, your outpatient clinic blocks include half days for independent learning, scholarly activity, and patient care support for your fellow residents’ patients. You will broaden your exposure to outpatient medicine by participating in specialty clinics, e.g. Gastroenterology, Nephrology, Endocrinology and Rheumatology. During the Ambulatory Care Rotation block (twice a year), you will also participate in the Women’s Health Clinic. Each clinic block includes a resident led Journal Club.
Your Outpatient Team:you will rotate with the same cohort of interns and residents during your clinic blocks. During your outpatient time, you will be supporting your colleagues who are not present in the clinic by assisting with their patient care tasks, to prevent gaps in patient care. You will be supported by faculty, nursing, social work for mental health, nutrition, a community health worker to assist with social determinants of health and our administrative staff.
Telemedicine: You will also have Telemedicine patient care sessions for patients who may not be able to physically come to the clinic. These occur by phone or video visit.
Ambulatory Care Rotation: sample schedule below.
| |
Monday |
Tuesday |
Wednesday |
Thursday |
Friday |
| AM |
Continuity Clinic |
Renal Clinic |
Neurology Clinic |
Journal Club followed by Continuity Clinic |
Continuity Clinic |
| PM |
Continuity Clinic |
Rheumatology Clinic |
Administrative Block |
Women’s Health Clinic |
Continuity Clinic |
Independent/Online Learning: in addition to your structured didactic sessions, we expect all residents to learn independently and develop lifelong learning skills. We have a variety of online resources on our residency webpage and provide time for study and scholarship. We also provide a 3 year ACP MKSAP board review subscription for all categorical residents.