

Systems & Computational Biology
Systems & Computational Biology: Seeing the Forest and the Trees
A decade ago, Einstein launched a systems and computational biology department—just the second of its kind in a U.S. medical school—to delve into the complexity of human biology
In the 1600s, the French philosopher Descartes posited that the world should be regarded somewhat like a clock: To comprehend it, one need only analyze the components and then reassemble them to recreate the whole. Descartes’ “reductionism,” as it came to be known, was profoundly influential, setting the stage for centuries of scientific discoveries in a variety of disciplines, including biology.
Department of Systems & Computational BiologyToday, biomedical scientists continue to dissect the components of the human body down to the molecular level, looking for clues to health and disease. However, scientists increasingly believe that many aspects of human biology are inextricably intertwined and can’t be fully understood by just examining their constituent parts.
Consider the Human Genome Project, which in 2003 finished sequencing and mapping every gene in our chromosomes. This monumental accomplishment was proclaimed as nature’s genetic blueprint for building a human being. But it was far from complete.
“Whether it’s statistically analyzing complex imaging or using mathematical modeling to explain unexpected findings, Aviv and his faculty bring a unique conceptual twist that elevates the rigor of my lab’s research and strengthens our results.”
– Paul Frenette, M.D.
“The map of the human genome does not necessarily explain how you go from genotype to phenotype—from an individual’s genes to his or her actual physical characteristics,” says Aviv Bergman, Ph.D., the Harold and Muriel Block Chair in Systems & Computational Biology and founding chair of the department. “While many physical traits arise from single genes, others result from many genes interacting with one another and with the environment. Out of that collective behavior you end up with what we call emergent properties—in this case, complex physical traits.”
Such traits include eye color, determined by the interaction of as many as 16 genes; and schizophrenia, a condition resulting from the interaction of hundreds of genes and untold epigenetic factors (non-genetic influences on gene expression).
As Aristotle wrote two millennia ago, “the whole is something over and above its parts and not just the sum of them all.”
A New Approach
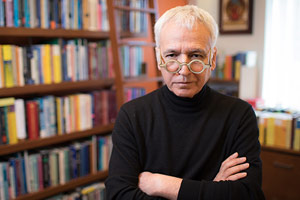
Aviv Bergman, Ph.D.Enter systems biology, a modern-day approach to understanding “the sum of them all.” It uses mathematical modeling (which explains things in terms of equations) and computational modeling (which uses computers to simulate the behavior of complex systems) to try to make sense of networks of molecules, genes, or cells—or even networks of networks (which is one way to describe a human being).
To Dr. Bergman, the key to understanding these networks is to decipher the “first principles” of biology—the fundamental rules that describe why biological systems behave the way they do. “An example of a first principle is the shape of the water molecule,” says Dr. Bergman. “The angle between the two hydrogen atoms is about 104 degrees. It’s never 90 or 180 degrees. This is a constraint imposed on the next layer of any biological system, so that anything that interacts with a water molecule has to abide by this physical reality.”
“Of course, that’s just a very basic example,” Dr. Bergman continues. “But as we learn the first principles of, say, how large numbers of genes interact, it’s not such a stretch to build a new understanding of how these interactions relate to yield complex traits including disease.”
“Our systems and computational biology colleagues have provided a stimulating new dimension to my department’s research. Their collaborative and creative approaches for tackling difficult questions in computational neuroscience have expanded and accelerated our research projects and afforded us new funding opportunities.”
– Kamran Khodakhah, Ph.D.
Dr. Bergman’s own research focuses on the evolution of robustness, a property that emerges within most systems where complex interactions occur among constituent parts. Robustness can be thought of as evolution’s way of ensuring the survival of an organism. In the context of genetics, robustness is controlled by interacting transcription factors (proteins that regulate gene expression), which effectively prevent the genetic system from undergoing significant change.
“Now, let’s apply this concept to cancer,” he says. “Cancer is typically seen as a cellular aberration stemming from a change in an oncogene or a tumor suppressor gene. But it may be more fruitful to look at cancer as a situation in which the mechanism of robustness—the checks and balances of a cell—has been broken. If one has a model of the robustness of a system, that gives you a mechanism to understand how this disruption occurred. In turn, one can potentially prevent the transition to metastasis and discover new therapeutic targets.”
Not Big Data
Systems biology, Dr. Bergman emphasizes, is not the same as “big data,” or large-scale number crunching—a common misperception.
“It is not about sequencing 10,000 genomes and deciphering the correlations between genes and disease,” he says. “That approach is still needed, but it is not what we as theoreticians will contribute. My goal is to create a prescriptive language, a mathematical language of sorts, that will enable us to talk about biology from a predictive point of view rather than a descriptive point of view.”

John Condeelis, Ph.D.Dr. Bergman adds that systems biology will not give us the “grand truth” about biology. “What we are doing is building models—reflections of reality that nicely match observations. We will never be able to fully simulate a patient. But we can get closer and closer to that goal by taking our models, testing them against experimental data and then refining those models as needed.”
Examples of how Einstein researchers are employing the tools of systems biology to understand disease are described below.
Hidden Figures: Clues to the Spread of Breast Cancer
How does breast cancer spread? It’s a crucial question, since most deaths from breast cancer and other types of cancer stem not from primary tumors but from cancer cells that have formed secondary growths elsewhere in the body—the process known as metastasis.
Using intravital imaging (which allows individual cells to be seen as they move through small sections of tumor tissue in living animals), Einstein researchers found that breast cancer metastasizes when three specific cells congregate. The place where this trio of cells meet is known as a tumor microenvironment of metastasis, or TMEM.
Featured Faculty
Assistant Professor
Systems & Computational Biology
Microbiology & ImmunologyDr. Kelly was a lead researcher on two recent and quite different papers. She found that the composition of people’s gut bacteria may explain why some of them suffer life-threatening reactions after taking a key metastatic colon cancer drug (npj Biofilms and Microbiomes November 2017). And she reported that a newly discovered family of viruses may play a key role in killing marine bacteria, thus influencing the ocean’s ecology (Nature January 2018).
Einstein Coverage
Previously Unknown Ocean Virus Family May Also Populate the Human Gut
Wednesday, January 24, 2018Gut Microbiome May Make Chemo Drug Toxic to Patients
Wednesday, November 01, 2017
TMEM are the sites where tumor cells enter blood vessels to commence their journey to distant regions of the body, says John Condeelis, Ph.D., professor and co-chair of anatomy and structural biology, co-director of the Gruss Lipper Biophotonics Center and the Judith and Burton P. Resnick Chair in Translational Research. By counting the number of TMEM in a breast-tissue sample, clinicians can estimate the likelihood that a patient’s cancer will spread. This has allowed Dr. Condeelis and colleagues to develop a TMEM test, which can yield vital information for treatment planning.
Analyzing the behavior of cells in the entire mammary gland, Dr. Condeelis suspected, might yield more information about metastasis—and improve the TMEM test. But there was one problem: “To see individual cells, you have to zoom in on a small fraction of the tumor,” he explains. “If you zoom out, you get the big picture but you lose the details.”
The solution, he realized, was to stitch together thousands of three-dimensional images, which would require mathematical wizardry and highly specialized tools such as support vector machine classifiers. Fortunately, one of the country’s few researchers who could apply this expertise was located one floor down in the Price Center/Block Pavilion: Aviv Bergman. Working together, Drs. Condeelis and Bergman figured out how to combine the images and make sense of the massive amount of data contained within.
It turns out that breast tumor cells tend to fall into one of two spatially segregated groups: fast-moving cells or slow-moving cells, which are associated with factors that promote metastasis and are located near blood vessels. Dr. Condeelis used this and other insights to determine that the fast-moving cells transform into slow ones as they approach a blood vessel, where the slow-moving cells deploy a finger-like protrusion to open a doorway into the bloodstream.
Dr. Condeelis used this new information to amend the TMEM test. “Now, we have a prognostic indicator that is 30 times better than the original test, with an accuracy rate of 92 percent, judging by initial clinical tests,” says Dr. Condeelis.
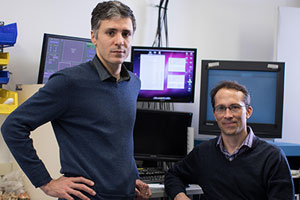
Ruben Coen-Cagli, Ph.D., Adam Kohn, Ph.D.The researchers also identified a receptor on macrophages (one of the cell types that make up a TMEM) that regulates the opening of the blood-vessel doorway. “In conjunction with Deciphera Pharmaceuticals, we collaboratively validated a drug that can inhibit this receptor,” says Dr. Condeelis. “It slams the door shut, preventing the dissemination of tumor cells.” The drug, rebastinib, is now being tested in a phase I clinical trial at Montefiore Health System.
In the Blink of an Eye
The modern era of vision research began in the late 1950s with David Hubel and Torsten Wiesel. They discovered how neurons are organized in the visual cortex and how similar visual neurons work together like tiny computational devices to relay information to the brain’s higher regions, where a visual image is formed and a visual memory stored.
“Without Ruben’s input, we would not be pursing many aspects of this research.”
– Adam Kohn, Ph.D.
Hubel and Torsten’s foundational work, which earned them a share of the 1981 Nobel Prize in Physiology or Medicine, was based on the response of small groups of neurons to simple images, such as moving lines. But their findings could not explain how the brain processes complex,real-world visual stimuli or how the brain uses ambiguous visual information to infer what’s in front of us. Those questions would await later generations of neuroscientists using more sophisticated tools.
One of those scientists is Adam Kohn, Ph.D., professor in the Dominick P. Purpura Department of Neuroscience, of ophthalmology & visual sciences, and of systems & computational biology and the Isidor Tachna Professor in Ophthalmology. Like Hubel and Wiesel, Dr. Kohn performs his experiments by recording the neuronal activity of animals as they are presented with visual stimuli. In his case, animals are presented with images that depict the natural world in a rich variety of shapes, patterns, textures, brightness levels and contrasts. Each test produces a vast amount of information, providing glimpses into how neurons form networks to process complex images.
Steven C. Almo, Ph.D.“Like so many other researchers, we’re drowning in data,” he says. “While these experiments do lead to new insights, we know that we’re missing a great deal.”
For help with finding what’s missing, Dr. Kohn has turned to Ruben Coen-Cagli, Ph.D., professor of systems & computational biology and in the Dominick P. Purpura Department of Neuroscience. Turning the conventional approach to biomedical discovery on its head, Dr. Coen-Cagli starts with theory and then tests it experimentally. “First, we generate hypotheses of how the brain might process visual information based on current biological knowledge,” he says. “Then, borrowing tools from artificial intelligence, computer science and machine learning, we develop algorithms [instructions for computers to follow] to perform object recognition and other image-processing tasks.”
Back in Dr. Kohn’s lab, the algorithms are tested against actual experimental data to see how well they can predict how the visual system will react to a given stimulus. “It’s a closed loop, where we go back and forth between theory and experimentation, making our models better and better,” says Dr. Coen-Cagli.
Featured Faculty
Assistant Professor
Systems & Computational Biology
Epidemiology & Population HealthDr. Mar was the driving force behind last summer’s first-ever Einstein hackathon. Forty-five “hackers” formed nine teams that competed to develop apps, websites and new ways to approach existing data on aging. Dr. Mar recently published two papers (PeerJ, May 2017; Methods, December 2017) assessing changes in the variability of gene expression, which can highlight important genes that are under different degrees of regulatory control.
Einstein Coverage
Einstein Tackles Aging at First-Ever Hackathon
Tuesday, August 08, 2017
“Our first goal,” he adds, “is to develop models that explain how the brain produces the vivid, coherent, and stable visual images that we experience in everyday life. And based on that understanding, we hope to advance technologies that could restore impaired vision and enhance normal vision.”
“Unlike most other research, ours is data validated rather than data driven,” Dr. Kohn explains. “Without Ruben’s input, we would not be pursuing many aspects of this research.”
Drug Design: By the Numbers
Drug discovery is an incredibly challenging enterprise. For every 10,000 compounds that show some potential in the laboratory, 250 reach preclinical (animal) testing, five advance to clinical trials, and one receives FDA approval.
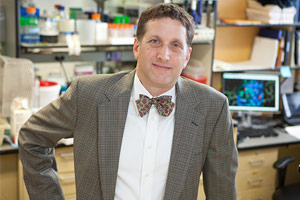
It’s no wonder that researchers are trying to improve the odds that a promising compound will find its way onto pharmacy shelves. One solution can be found in the field of systems and computational biology, according to Steven C. Almo, Ph.D., professor and chair of biochemistry, professor of physiology & biophysics and the Wollowick Family Foundation Chair in Multiple Sclerosis and Immunology.
A structural biologist, Dr. Almo studies the shape of proteins. “Knowing a protein’s shape provides a blueprint for its function,” he says. “And once you understand its function, you can modify its activity to treat disease.”

Andras Fiser, Ph.D.Dr. Almo is particularly interested in proteins on the surface of T cells—immune cells that recognize and destroy cells infected by pathogens or that have become cancerous. These surface proteins on T cells are receptors that serve as sentries: When the receptors recognize tell-tale proteins on a diseased cell, they turn on the T cells and accelerate their activity.
Sometimes T cells don’t work as well as they should (letting microbes or malignancies run wild) or work too well (causing autoimmune disease through an overzealous response to the body’s own tissues). Dr. Almo’s goal is to fine-tune T-cells to destroy disease-causing cells without damaging healthy tissue. He does so by designing drugs that control T-cell function by acting as ligands: molecules that engage with and activate T-cell receptors, much like a key fitting into and opening a lock. These synthetic ligands could ramp up or tamp down T-cell activity as needed.
Dr. Almo first determines the receptor’s shape by using X-ray crystallography: forming crystals of the receptor into a crystal and exposing them to an X-ray beam. “The crystals diffract, or bend, the beam, and you get a beautiful diffraction pattern,” he says. “From that diffraction pattern, you can determine the structure of that molecule in exquisite detail, revealing every atom.”
“We go back and forth between our labs. Using Andras’ data to inform my experiments, which he then uses to improve his models. It’s a beautiful synergy between computation and experiment.”
– Steven C. Almo, Ph.D.
X-ray crystallography suggests the shape that a ligand for activating the receptor should take. But a lot of work remains, since receptors are large, complex molecules, and ligands must engage multiple receptors to activate a T cell. The number of structural permutations that ligands can take are enough to boggle the mind—but not a computer.
To add more precision to the drug-design process, Dr. Almo regularly turns to Andras Fiser, Ph.D., professor of systems & computational biology and of biochemistry, who is able to assign a number to almost every nook and cranny of a protein.
“Once we analyze a receptor protein, we can develop algorithms to model how the receptor and a potential ligand will interact, how tightly they bind and whether the receptor can bind multiple ligands,” says Dr. Fiser. “When we have that information, we can embark on designing ligands that possess the desired specificities.”
Yinghao Wu, Ph.D.Such in silico (“in computer”) experiments dramatically reduce the number of actual lab experiments that need to be conducted, which saves Dr. Almo both time and resources. “We go back and forth between our labs,” says Dr. Almo, “using Andras’ data to inform my experiments, which he then uses to improve his models. It’s a beautiful synergy between computation and experiment.”
Dr. Almo also collaborates with Yinghao Wu, Ph.D., assistant professor of systems & computational biology—in this case, to turn on the desired types of T cells. In recent years, the U.S. Food and Drug Administration has approved a number of immunotherapy drugs that treat cancer by regulating T cell activity. The drugs can be quite effective but often cause significant side effects. “The problem is that these drugs tend to affect all T cells,” says Dr. Almo. “Combined with our experimental approaches, Yinghao’s computations show us how to home in on just the disease-relevant T cells, reducing off-target effects.”
From Descartes to Darwin
Systems biology remains the exception, not the rule, despite its tremendous potential. Only a few medical schools have departments dedicated to the field, and NIH funding still goes mainly to the study of individual trees, not the forest. But Dr. Kohn, for one, is optimistic that biologists will realize that more data isn’t necessarily the answer. “Look at Darwin,” he says. “He didn’t catalog millions of examples and come up with the idea of evolution. He was looking for general principles and used a handful of observations to get to his grand theory.”
Posted on: Wednesday, April 18, 2018




