Research Highlights
Curbing Cervical Cancer
Great progress has been made against cervical cancer, due mainly to better prevention, screening and treatment—and Albert Einstein Cancer Center researchers have played active roles in all of these areas.
The Vaccines
This article originally appeared in the Winter/Spring issue of the Einstein Cancer Center newsletter.Some 13 different types of human papillomavirus (HPV) cause cervical cancer, but just two are responsible for most cases: HPV16 (50 percent of cases) and HPV18 (10 percent). Today, two cervical cancer vaccines—Cervarix and Gardasil—protect against HPV16 and HPV18. How do they compare?
"The College of Medicine was the lead site in a postmarketing clinical trial of these vaccines and found stronger immunity with Cervarix," says Dr. Mark Einstein, associate professor of obstetrics & gynecology and women's health at Einstein. But Gardasil has an added virtue: It not only prevents cervical cancer; it also protects against genital warts by targeting two other viruses, HPV6 and HPV11. His conclusion: Both vaccines work and can spare women from potentially debilitating disease. "My daughters will be getting the vaccine when they come of age," says Dr. Einstein, also director of clinical research for women's health and gynecologic oncology at Montefiore, the University Hospital and academic medical center for Einstein.
Remaining Challenges
Much work remains to be done if we are to make cervical cancer a disease of the past. Getting more girls vaccinated should be a top priority.

Nicolas F. Schlecht, Ph.D.The Centers for Disease Control and Prevention recommends the vaccine for all girls ages 11 and 12. Yet only half of all American girls are getting it, many not early enough. Einstein's Dr. Nicolas F. Schlecht and colleagues detected HPV DNA in 59 percent of cervical samples from 97 sexually active, inner-city adolescent minority women who had not been vaccinated, meaning the adolescents had already been exposed and infected. By contrast, in another study that included 327 fully vaccinated adolescents, the number of cervical samples positive for HPV was as much as 80 percent lower, depending on the type of HPV. These studies illustrate the urgency of the need for early vaccination, says Dr. Schlecht, associate professor of epidemiology & population health and of medicine.
Tackling the Problem of HIV and HPV
Dr. Kathryn Anastos, co-director of the Einstein Global Health Center, studies cervical cancer risk worldwide in women with HIV. In research conducted with Dr. Einstein, Dr. Robert D. Burk and Dr. Howard D. Strickler, she found that women infected with HIV—the human immunodeficiency virus, which causes AIDS—are more likely to have high-risk, and multiple types of, HPV infection and cervical precancer. An organization that she co-founded in 2004 in Rwanda, the Women's Equity in Access to Care and Treatment for HIV, brings antiretroviral drugs and cervical cancer screening to HIV-positive women.

Kathryn Anastos, M.D.Dr. Strickler heads HPV research in the Women's Interagency HIV Study (WIHS). This study followed more than 3,000 HIV-infected and 1,000 uninfected women for more than a decade. It is the most comprehensive prospective investigation of the natural history of HPV infection and precancer/cancer development in HIV-positive women. This study has played a major role in defining cancer screening guidelines. Dr. Strickler is also co-leader of the AECC's Cancer Epidemiology Program.
Dr. Einstein is also the principal investigator of a National Cancer Institute (NCI)-funded trial being carried out at four large African hospitals. Women with cervical cancer and HIV infection will be treated with a combination of radiation and chemotherapy. And through Dr. Anastos' NCI-funded education grant, African scientists and healthcare professionals come to Einstein for training in various aspects of clinical and epidemiological research.
Screening and Treatment
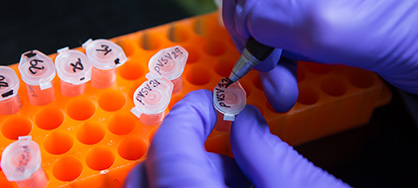
Looking for changes in tumor cells. So-called epigenetic changes are normal ways by which a cell's gene expression is controlled. The most common epigenetic changes involve molecules called methyl groups that attach to and silence genes. Cancer can develop if methyl groups silence tumor-suppressor genes that help keep cancerous cells in check. Dr. Einstein and his colleagues are studying patients at Montefiore and Jacobi Medical Centers who have persistent HPV infection and early precancerous cervical lesions to see if methylation patterns in the cervical cells predict which lesions are likely to develop into cancer.

Mark H. Einstein, M.D., M.S. '05; Robert D. Burk, M.D.; and Howard D. Strickler, M.D.Looking for changes in viruses. Dr. Burk and his colleagues examined methylation patterns in the genomes of HPV viral types that cause most cases of cervical cancer. In a 2012 study in the Journal of the National Cancer Institute, the researchers reported higher HPV DNA methylation in women with precancerous cervical lesions compared to women with the same HPV type but no detectable precancerous cells. The findings suggest that HPV viral methylation can be useful in identifying which HPV cervical infections may lead to cancer. Dr. Burk is professor of pediatrics (genetics), of microbiology & immunology, of obstetrics & gynecology and women's health, and of epidemiology & population health.
How viruses slip under the radar. Einstein scientists led by Dr. Strickler found that HIV-positive women have a low immune-system response to HPV16, suggesting that the virus has developed a way to avoid immune system surveillance. The researchers are looking for genetic and epigenetic (gene-expression) factors that give the virus this "invisibility cloak."
Molecular methods for cervical cancer screening. A new four-year study led by Dr. Strickler and involving Drs. Burk, Einstein and Anastos will examine the use of molecular methods to identify HPV and cellular factors that can improve the accuracy of cervical cancer screening in HIV-positive women. The NCI-supported study follows a 2012 paper published in the Journal of the American Medical Association by the team suggesting that HPV DNA testing can help reduce the frequency of Pap testing in HIV-positive women.
HIV, aging and immune status. Because antiretroviral therapy has been so successful, more HIV-positive women now live to the ages when cervical cancer rates peak. Dr. Strickler recently received an NIH grant to explore:
- how menopause and HIV affect HPV infection and development of early cervical lesions;
- what immune deficits drive the relationship of HIV with cervical cancer and thus can be targeted in prevention and treatment;
- which genes govern the interaction between the immune system and abnormal cervical cells.
A better treatment regimen. Cisplatin is an effective cancer chemotherapy drug. But if cervical cancer recurs and cisplatin has already been used, only 13 percent of patients respond to the drug. Dr. Einstein and Dr. Dennis Kuo, professor of clinical obstetrics & gynecology and women's health, found that the combination of paclitaxel and oxaliplatin—two other anticancer agents—is effective in treating patients with recurrent cervical cancer who have previously been exposed to cisplatin.
Posted on: Monday, July 01, 2013

Who should get vaccinated against HPV infection?
The vaccines are not just for preventing cervical cancer in girls and women ages 9 through 26. One of the two vaccines, Gardasil, also protects against genital warts and anal cancer in men as well as women, and the U.S. Centers for Disease Control recommends that males be vaccinated with Gardasil at age 11 or 12.